The cheeks contain the buccinator muscle, which, along with the tongue, holds food between the teeth during mastication.
The palate forms both the roof of the oral cavity and the floor of the nasal cavity and consists of a hard and a soft palate.
All the muscles that act upon the soft palate are innervated by the vagus nerve [cranial nerve (CN) X], with the exception of the tensor veli palatini, which is innervated by a small motor branch from CN V-3. The difference in innervation reflects the embryologic origins of the branchial arches.
Hard Palate
The hard palate consists of the palatine process of the maxillary bone and the horizontal plate of the palatine bone (Figure 24-1A and B). 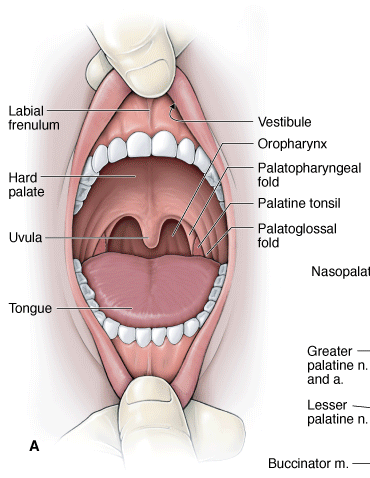
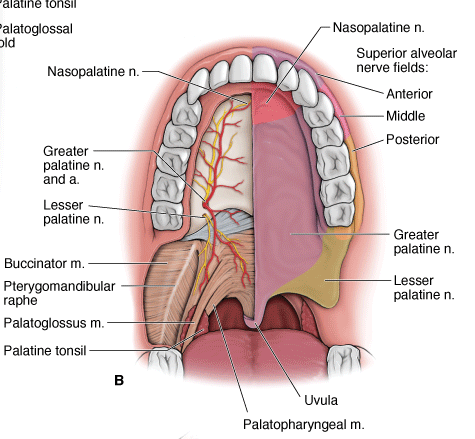
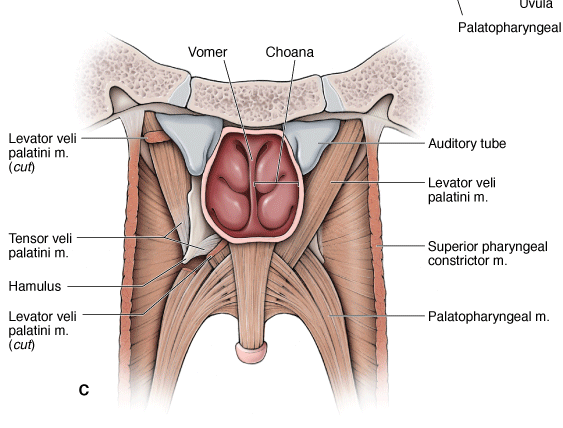
A. Open mouth showing the palatal arches. B. Anterior view of the innervation of the palate. C. Posterior view of the palate.
The incisive canal is in the anterior midline and transmits the following branches (Figure 24-1B):
- Nasopalatine and greater palatine nerves. Branches of the maxillary nerve (CN V-2); provides general sensation to the palate.
- Sphenopalatine and greater palatine arteries. Branches of the maxillary artery originating from the infratemporal fossa.
Soft Palate
The soft palate forms the soft, posterior segment of the palate. The soft palate has a structure called the uvula, which is suspended from the midline (Figure 24-1A–C). The soft palate is continuous with the palatoglossal and palatopharyngeal folds. Functionally, the soft palate ensures that food moves inferiorly down into the esophagus when swallowing, rather than up into the nose. By moving posteriorly against the pharynx, which separates the oropharynx from the nasopharynx, the soft palate acts like a flap valve. The vascular supply is bilaterally derived from the lesser palatine artery (maxillary artery) and from smaller arteries, including the ascending palatine artery of the facial artery and the palatine branch of the ascending pharyngeal artery. The soft palate receives general sensory innervation via the lesser palatine nerves (CN V-2) (Figure 24-1B).
Muscles of the Soft Palate
The muscles of the soft palate are as follows (Figure 24-1B and C):
- Tensor veli palatini muscle. Attaches laterally to the pterygoid plate of the sphenoid bone, hooks around the hamulus, and inserts in the soft palate. This muscle is innervated by CN V-3. As its name implies, contraction results in tensing the soft palate.
- Levator veli palatini muscle. Originates along the cartilaginous portion of the auditory tube and inserts into the superior aspect of the soft palate. Contraction of this muscle elevates the soft palate and is innervated by CN X.
 To test the function of CN X, the physician will ask the patient to open his mouth wide to determine if the palate deviates to one side or the other during a yawning motion. A lesion of CN X causes paralysis of the ipsilateral levator veli palatini muscle, resulting in the uvula being pulled superiorly to the opposite side of the lesion.
To test the function of CN X, the physician will ask the patient to open his mouth wide to determine if the palate deviates to one side or the other during a yawning motion. A lesion of CN X causes paralysis of the ipsilateral levator veli palatini muscle, resulting in the uvula being pulled superiorly to the opposite side of the lesion.
- Palatoglossus muscle. Attaches between the soft palate and the tongue and is innervated by CN X. The palatoglossus muscle and the palatopharyngeus muscle surround the palatine tonsil, which aids the immune system in combating pathogens entering the oral cavity.
 Inflammation of the palatine tonsils (tonsillitis) is associated with difficulty swallowing and sore throat. Because the palatine tonsils are visible when inspecting the oral cavity, the tonsils of a patient who has tonsillitis will appear enlarged and red. In cases of chronic tonsillitis, the tonsils may be surgically removed (tonsillectomy) to ensure that the patient can swallow and breathe properly.
Inflammation of the palatine tonsils (tonsillitis) is associated with difficulty swallowing and sore throat. Because the palatine tonsils are visible when inspecting the oral cavity, the tonsils of a patient who has tonsillitis will appear enlarged and red. In cases of chronic tonsillitis, the tonsils may be surgically removed (tonsillectomy) to ensure that the patient can swallow and breathe properly.
The tongue consists of skeletal muscle, which has a surface covered with taste buds (special sensory) and general sensory nerve endings. The tongue is supported in the oral cavity by muscular connections to the hyoid bone, mandible, styloid process, palate, and pharynx. The V-shaped sulcus terminalis divides the tongue into anterior and posterior divisions, which differ developmentally, structurally, and by innervation. The foramen cecum is located at the apex of the “V” and indicates the site of origin of the embryonic thyroglossal duct.
Tongue muscles are bilaterally paired and innervated by the hypoglossal nerve (CN XII) (Figure A and C):
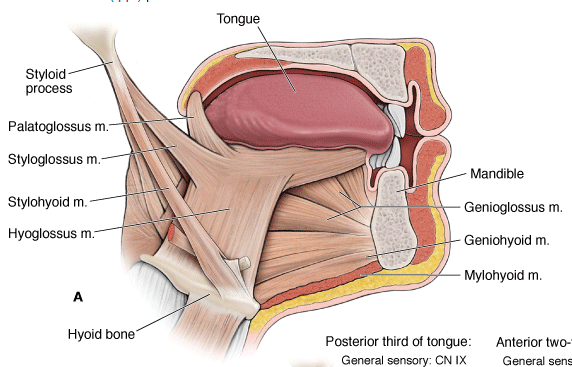
- Genioglossus muscle. Attaches between the internal surface of the mandible and the tongue. Contraction causes the tongue to protrude out of the oral cavity (“sticking out your tongue”).
- Hyoglossus muscle. Courses lateral to the genioglossus muscle, with attachments from the hyoid bone to the tongue. The lingual artery, en route to the tongue, courses between the hyoglossus and genioglossus muscles. In contrast, CN XII and CN V-3 course from the infratemporal fossa to the tongue, along the external surface of the hyoglossus muscle.
- Styloglossus muscle. Originates on the styloid process of the temporal bone and courses between the superior and middle pharyngeal constrictors to insert on the lateral surface of the tongue.
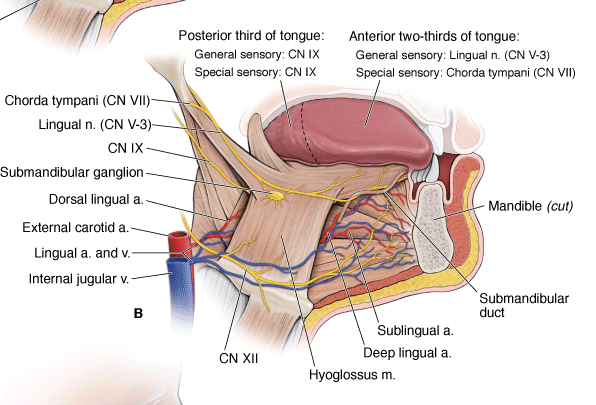
A. Tongue muscles. B. Neurovascular supply of the tongue. C. Innervation of the tongue.
The following nerves innervate the tongue:
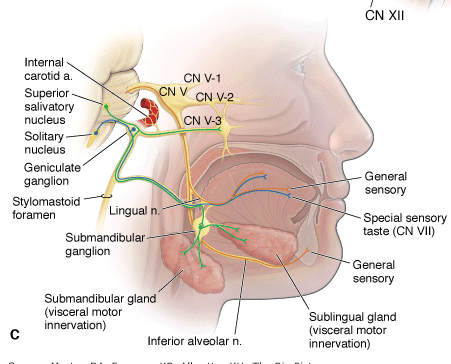
- CN V-3 (lingual nerve). The anterior two-thirds of the tongue receives its general sensory innervation from the lingual branch of CN V-3. The submandibular duct ascends from the submandibular gland to open adjacent to the lingual frenulum. The lingual nerve courses inferior to the submandibular duct.
- CN VII (facial nerve). The anterior two-thirds of the tongue receives its special sensory (taste) innervation from the chorda tympani nerve (CN VII).
- CN IX (glossopharyngeal nerve). The posterior third of the tongue receives both its general sensory and special sensory (taste) innervation from CN IX.
- CN XII (hypoglossal nerve). All of the tongue muscles receive their somatic motor innervation via CN XII (except the palatoglossus, which is innervated by CN X).
 To clinically test CN XII, the physician will ask the patient to stick out her tongue. If CN XII is functioning normally, the tongue should extend out evenly in the midline. If there is a lesion of CN XII, the tongue will deviate toward the same side of the face as the lesion. An easy way to remember this is that a lesion of CN XII will cause the patient to “lick her wounds.”
To clinically test CN XII, the physician will ask the patient to stick out her tongue. If CN XII is functioning normally, the tongue should extend out evenly in the midline. If there is a lesion of CN XII, the tongue will deviate toward the same side of the face as the lesion. An easy way to remember this is that a lesion of CN XII will cause the patient to “lick her wounds.”
The lingual artery arises from the external carotid artery at the level of the tip of the greater horn of the hyoid bone in the carotid triangle. The lingual artery courses anteriorly between the hyoglossus and the genioglossus muscles, giving rise to the dorsal lingual and sublingual branches and terminating as the deep lingual artery.
Content 3
Saliva is essential for maintaining healthy oral tissue. It is composed primarily of water as well as mucins, enzymes, and antibodies. Saliva initiates the chemical digestion of carbohydrates (the enzyme salivary amylase) and lubricates masticated food into a bolus. The three glands that produce saliva are the parotid, submandibular, and sublingual glands.
The 2 main types of salivary glands are the major salivary glands and minor salivary glands.
There are 3 sets of major salivary glands on each side of the face:
- The parotid glands, the largest salivary glands, are just in front of the ears. About 7 out of 10 salivary gland tumors start here. Most of these tumors are benign but the parotid glands still are where most malignant (cancerous) salivary gland tumors start.
- The submandibular glands are smaller and are below the jaw. They secrete saliva under the tongue. About 1 or 2 out of 10 tumors start in these glands, and about half of these tumors are cancer.
- The sublingual glands, which are the smallest, are under the floor of the mouth and below either side of the tongue. Tumors starting in these glands are rare.
Ductual Openings into the Oral Cavity
The bilateral openings of ducts of the salivary glands into the oral cavity are as follows:
- Parotid gland. The duct opens opposite the second maxillary molar.
- Submandibular gland. The duct courses medial to the lingual nerve and opens into the area adjacent to the lingual frenulum (Figure 24-2B).
- Sublingual gland. The duct opens at the base of the tongue.
Innervation of the Salivary Glands
The parasympathetic nervous system is responsible for providing visceral motor innervation to the salivary glands via the following cranial nerves (Figure 24-2C):
- Parotid gland. CN IX, via the otic ganglion.
- Submandibular gland. CN VII, via the submandibular ganglion.
- Sublingual gland. CN VII, via the submandibular ganglion.
The teeth cut, grind, and mix food during mastication.
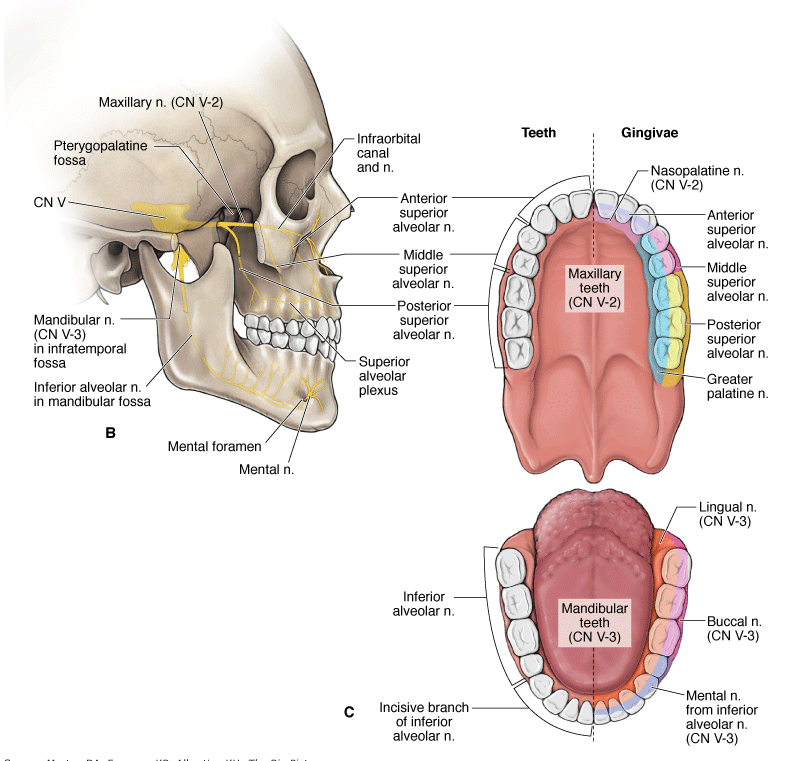
In adults, there are 16 teeth in the maxilla and 16 in the mandible. Branches of CN V-2 and the maxillary artery and veins supply the maxillary teeth and gingivae. Branches of CN V-3, and the inferior alveolar artery and veins supply the mandibular teeth and gingivae.
Types of Teeth
There are 20 teeth in a child and 32 in an adult. Adult teeth are typically numbered in a progressing clockwise fashion, with tooth number 1 (upper right maxillary molar) across to tooth number 16 (upper left maxillary molar). Tooth number 17 is the left third mandibular molar and continues to tooth number 32, the right third mandibular molar (Figure 24-3A).
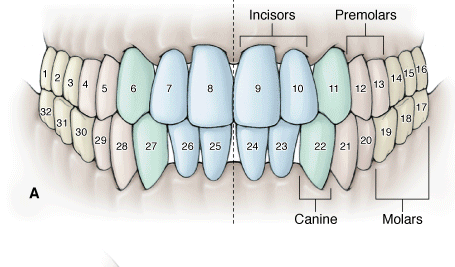 The teeth are divided into four quadrants with eight teeth located in the upper left, upper right, lower left, and lower right halves of the maxilla and mandible. Each quadrant consists of the following teeth:
The teeth are divided into four quadrants with eight teeth located in the upper left, upper right, lower left, and lower right halves of the maxilla and mandible. Each quadrant consists of the following teeth:
- Two Incisors. Chisel-shaped teeth ideal for cutting or biting. There is a central and a lateral incisor.
- One Canine. A single pointed tooth used for tearing food.
- Two Premolars. Have two cusps, which are used for grinding.
- Three Molars. Have three cusps, which also are used for grinding. The third and most posterior molar tooth emerges last, usually in the late adolescent years, and is often referred to as the wisdom tooth.
Cavities (dental carries) are holes in the teeth. Cavities form through the deposit of food products on teeth, known as plaque. Bacteria inhabit the plaque and metabolize carbohydrates into acids. Over time, the acids dissolve the outer protection of the tooth, the enamel, resulting in cavities.
The innervation of the teeth and gingivae are as follows (Figure 24-3B and C):
- Maxillary teeth. CN V-2 enters the pterygopalatine fossa via the foramen rotundum. CN V-2 branches provide general sensory innervation to the maxillary teeth in a plexus of nerves formed by the anterior, middle, and posterior superior alveolar nerves.
- Maxillary gingivae. The posterior, middle, and anterior superior alveolar nerves innervate the buccal surface of the gingivae, whereas the greater palatine and nasopalatine nerves innervate the lingual surface.
- Mandibular teeth. CN V-3 enters the infratemporal fossa via the foramen ovale. A branch of CN V-3, the inferior alveolar nerve, enters the mandibular foramen and provides general sensory innervation to the teeth on that side of the mandible. The inferior alveolar nerve exits the mandibular canal as the mental nerve by traversing the mental foramen and providing general sensory innervation to the bottom lip.
- Mandibular gingivae. The buccal and mental nerves innervate the buccal surface of the gingivae, whereas the lingual nerve innervates the lingual surface.
 An inferior alveolar nerve block is administered to patients who require dental work in the mandible. Injection of local anesthetics (e.g.,
lidocaine) into the oral mucosa at the lingula of the mandible will anesthetize the inferior alveolar nerve and potentially the proximal lingual nerve, resulting in numbness of the tongue and oral mucosa. Care must be given when extracting the third molar tooth because the lingual nerve is closely associated with this nerve.
An inferior alveolar nerve block is administered to patients who require dental work in the mandible. Injection of local anesthetics (e.g.,
lidocaine) into the oral mucosa at the lingula of the mandible will anesthetize the inferior alveolar nerve and potentially the proximal lingual nerve, resulting in numbness of the tongue and oral mucosa. Care must be given when extracting the third molar tooth because the lingual nerve is closely associated with this nerve.
 A plexus formed by the anterior superior, middle superior, and posterior superior alveolar nerves supplies the maxillary teeth. Unlike the mandibular teeth, where anesthesia can be administered in one location to effectively block all the teeth on that side, the maxillary teeth must be considered separately. The palate must also be considered; therefore, a greater palatine as well as a nasopalatine nerve block is often administered during dental procedures.
A plexus formed by the anterior superior, middle superior, and posterior superior alveolar nerves supplies the maxillary teeth. Unlike the mandibular teeth, where anesthesia can be administered in one location to effectively block all the teeth on that side, the maxillary teeth must be considered separately. The palate must also be considered; therefore, a greater palatine as well as a nasopalatine nerve block is often administered during dental procedures.
- Maxillary molars. Injection is given at the region of the second molar.
- Maxillary premolars. Injection is given at the region of the second premolar.
- Maxillary canine and incisors. Injection can be given above the roots of the anterior teeth or via an infraorbital nerve block.

The arteries supplying the teeth mirror their accompanying nerves.
- Posterior superior alveolar artery. Originates from the infraorbital artery, which arises from the maxillary artery in the pterygopalatine fossa. The infraorbital artery exits the fossa and enters the infraorbital canal, where branches supply the maxillary molars and premolars.
- Anterior superior alveolar artery. Originates from the infraorbital artery, where branches course through the maxilla to supply the incisor and canines.
- Inferior alveolar artery. Originates from the maxillary artery and courses with the inferior alveolar nerve through the mandibular canal to supply the mandibular teeth.
Veins from the maxillary and mandibular teeth generally mirror the arteries.
References