Update November 22, 2018

Cross section of the eyelids. (Courtesy of C Beard.)
The orbits are related to the frontal sinus above, the maxillary sinus below, and the ethmoid and sphenoid sinuses medially.
The thin orbital floor is easily damaged by direct trauma to the globe, resulting in a “blowout” fracture with herniation of orbital contents into the maxillary antrum. Infection within the sphenoid and ethmoid sinuses can erode the paper-thin medial wall (lamina papyracea) and involve the contents of the orbit. Defects in the roof (eg, neurofibromatosis) may result in visible pulsations of the globe transmitted from the brain.
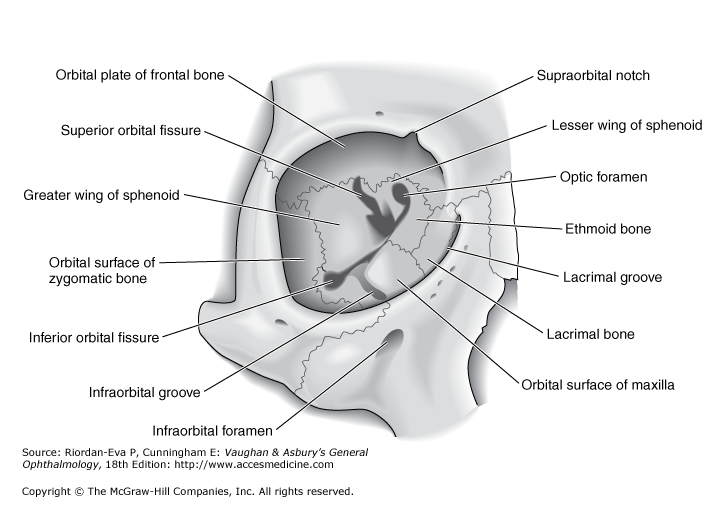
Anterior view of bones of right orbit.
[The eyeball is within a bony protective orbital encasement. It is composed of the following structures:

A. Bony orbit. B. Lacrimal apparatus. C. Sagittal section of the eyelid. D. A normal right eye in contrast to an eye with Horner's syndrome.]
The orbit is bordered superiorly by the frontal bone and the lesser wing of the sphenoid bone. Supraorbital foramen. Transmits the supraorbital nerve [cranial nerve (CN) V-1] and vessels to the scalp.
Lateral wall is formed by the zygomatic bone and the greater wing of the sphenoid bone.
Formed by the maxillary, zygomatic, and palatine bones.
- Infraorbital foramen. Transmits the infraorbital nerve (CN V-2) and vessels to the maxillary region of the face.
The medial walls of the right and left orbit are parallel and are separated by the nose.
In each orbit, the lateral and medial walls form an angle of 45°, which results in a right angle between the two lateral walls. The orbit is compared to the shape of a pear, with the optic nerve representing its stem. The anterior circumference is somewhat smaller in diameter than the region just within the rim, which makes a sturdy protective margin.
The medial wall is formed by the ethmoid, frontal, lacrimal, and sphenoid bones.
- Anterior and posterior ethmoidal foramina. Transmits the anterior and posterior ethmoidal nerves and vessels, to the nasal cavity and the sphenoid and ethmoid sinuses.
- Nasolacrimal canal. Formed by the maxillary, lacrimal, and inferior nasal concha bones. Drains tears from the eye to the inferior meatus in the nasal cavity.
medially by the ethmoid sinus, inferiorly by the maxillary sinus, and laterally by the zygomatic bone. See Figure below. The roof of the orbit is composed principally of the orbital plate of the frontal bone. The ethmoid bone (lamina papyracea) is paper thin and is the most likely sinus wall to break in blunt eye trauma or to be perforated due to sinusitis with subsequent spread of infection to the orbit. The orbital contents include the ocular muscles retroseptal fat and optic nerve, whereas the globe is considered a separate entity.

Medial view of bony wall of left orbit.
Optic canal. Transmits the optic nerve (CN II) and the ophthalmic artery.
- Superior orbital fissure. An opening between the greater and lesser wings of the sphenoid bone that transmits the oculomotor, trochlear, ophthalmic, and abducens nerves (CNN III, IV, V-1, and VI, respectively), and the ophthalmic veins.
- Inferior orbital fissure. Communicates with the infratemporal and pterygopalatine fossae. The inferior orbital fissure transmits CN V-2 and the infraorbital artery and vein.
Roof
The lacrimal gland is located in the lacrimal fossa in the anterior lateral aspect of the roof. Posteriorly, the lesser wing of the sphenoid bone containing the optic canal completes the roof. {Defects in the roof (eg, neurofibromatosis) may result in visible pulsations of the globe transmitted from the brain.}
Floor
The floor of the orbits is composed of the maxillary sinus below, and the ethmoid and sphenoid sinuses medially. The thin orbital floor is easily damaged by direct trauma to the globe, resulting in a "blowout" fracture with herniation of orbital contents into the maxillary antrum.
{Infection within the sphenoid and ethmoid sinuses can erode the paper-thin medial wall (lamina papyracea) and involve the contents of the orbit.}
==============================
The anterior limit of the orbital cavity is the orbital septum, which acts as a barrier between the eyelids and orbit.
The lateral wall is separated from the roof by the superior orbital fissure, which divides the lesser from the greater wing of the sphenoid bone. The anterior portion of the lateral wall is formed by the orbital surface of the zygomatic (malar) bone. This is the strongest part of the bony orbit. Suspensory ligaments, the lateral palpebral tendon, and check ligaments have connective tissue attachments to the lateral orbital tubercle.
The orbital floor is separated from the lateral wall by the inferior orbital fissure. The orbital plate of the maxilla forms the large central area of the floor and is the region where blowout fractures most frequently occur. The frontal process of the maxilla medially and the zygomatic bone laterally complete the inferior orbital rim. The orbital process of the palatine bone forms a small triangular area in the posterior floor.
The boundaries of the medial wall are less distinct. The ethmoid bone is paper-thin but thickens anteriorly as it meets the lacrimal bone. The body of the sphenoid forms the most posterior aspect of the medial wall, and the angular process of the frontal bone forms the upper part of the posterior lacrimal crest. The lower portion of the posterior lacrimal crest is made up of the lacrimal bone. The anterior lacrimal crest is easily palpated through the lid and is composed of the frontal process of the maxilla. The lacrimal groove lies between the two crests and contains the lacrimal sac.
Orbital Apex
The apex of the orbit is the main portal for all nerves and vessels to the eye and the site of origin of all extraocular muscles except the inferior oblique. The superior orbital fissure lies between the body and the greater and lesser wings of the sphenoid bone. The superior ophthalmic vein and the lacrimal, frontal, and trochlear nerves pass through the lateral portion of the fissure that lies outside the annulus of Zinn. The superior and inferior divisions of the oculomotor nerve and the abducens and nasociliary nerves pass through the medial portion of the fissure within the annulus of Zinn. The optic nerve and ophthalmic artery pass through the optic canal, which also lies within the annulus of Zinn. The inferior ophthalmic vein frequently joins the superior ophthalmic vein before exiting the orbit. Otherwise, it may pass through any part of the superior orbital fissure, including the portion adjacent to the body of the sphenoid that lies inferomedial to the annulus of Zinn, or through the inferior orbital fissure.
Blood Supply
The principal arterial supply of the orbit and its structures derives from the ophthalmic artery, the first major branch of the intracranial portion of the internal carotid artery. This branch passes beneath the optic nerve and accompanies it through the optic canal into the orbit. The first intraorbital branch is the central retinal artery, which enters the optic nerve about 8–15 mm behind the globe. Other branches of the ophthalmic artery include the lacrimal artery, supplying the lacrimal gland and upper eyelid; muscular branches to the various muscles of the orbit; long and short posterior ciliary arteries; medial palpebral arteries to both eyelids; and the supraorbital and supratrochlear arteries. The short posterior ciliary arteries supply the choroid and parts of the optic nerve. The two long posterior ciliary arteries supply the ciliary body and anastomose with each other and with the anterior ciliary arteries to form the major arterial circle of the iris. The anterior ciliary arteries are derived from the muscular branches to the rectus muscles. They supply the anterior sclera, episclera, limbus, and conjunctiva and contribute to the major arterial circle of the iris. The most anterior branches of the ophthalmic artery contribute to the formation of the arterial arcades of the eyelids, which make an anastomosis with the external carotid circulation via the facial artery.
The venous drainage of the orbit is primarily through the superior and inferior ophthalmic veins, into which drain the vortex veins, the anterior ciliary veins, and the central retinal vein. The ophthalmic veins communicate with the cavernous sinus via the superior orbital fissure and the pterygoid venous plexus via the inferior orbital fissure. The superior ophthalmic vein is initially formed from the supraorbital and supratrochlear veins and from a branch of the angular vein, all of which drain the skin of the periorbital region. This provides a direct communication between the skin of the face and the cavernous sinus, thus forming the basis of the potentially lethal cavernous sinus thrombosis, secondary to superficial infection of the periorbital skin.
The anterior circumference is somewhat smaller in diameter than the region just within the rim, which makes a sturdy protective margin.
The lacrimal apparatus keeps the eye moist and free of dust and other irritating particles through the production and drainage of tears.
The lacrimal gland lies in the superolateral corner of the orbit.
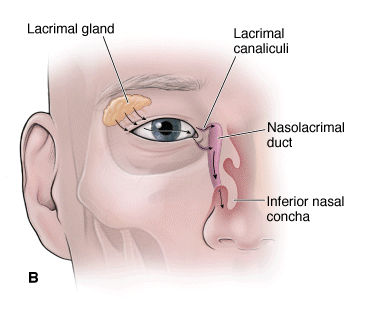
- Tears. The lacrimal gland secretes tears that spread evenly over the eyeball through blinking and cleanse the eye of dust and foreign particles.
- Drainage. Tears drain from the eyeball, via the nasolacrimal duct, into the inferior nasal meatus of the nasal cavity.
- Innervation. The lacrimal gland is innervated by visceral motor parasympathetic neurons from CN VII (Figure 18-4C).
 Because the mucosa of the nasal cavity is continuous with the mucosa of the nasolacrimal duct system, a cold or “stuffy” nose often causes the lacrimal mucosa to become inflamed and swollen. Swelling constricts the ducts and prevents tears from draining from the eye surface, causing “watery” eyes.
Because the mucosa of the nasal cavity is continuous with the mucosa of the nasolacrimal duct system, a cold or “stuffy” nose often causes the lacrimal mucosa to become inflamed and swollen. Swelling constricts the ducts and prevents tears from draining from the eye surface, causing “watery” eyes.
Eyelids protect the eye from foreign particles and from bright light.
Landmarks
The normal eyelid crease is 6 to 7 mm away from the eyelid margin in adults. This crease is not appreciable in most Asian eyelids. The upper eyelid normally covers the top 1 mm of the cornea, and the lower eyelid typically lies at the junction of the cornea and sclera
Normal eyelid positionThe upper lid covers 1 to 2 mm of the upper limbus. The lower lid covers the lower limbus minimully. The central light reflex can be seen within the pupil. The margin reflex distance is measured from this reflex to the upper eyelid margin..
The palpebral fissure (PF) represents the distance between the upper and lower eyelid margins at the axis of the pupil. The normal PF measures 9 to 12 mm.
A point source of light directed at the patient creates a central pupillary light reflex. The distance from this reflex to the upper eyelid margin is called the margin reflex distance (MRD). Normally this measures 4 to 5 mm. Margin reflex distance is often more helpful than PF since lower lid position may vary individually.
The PF and MRD provide an objective means of identifying ptosis and measuring its severity that may be useful in planning treatment.
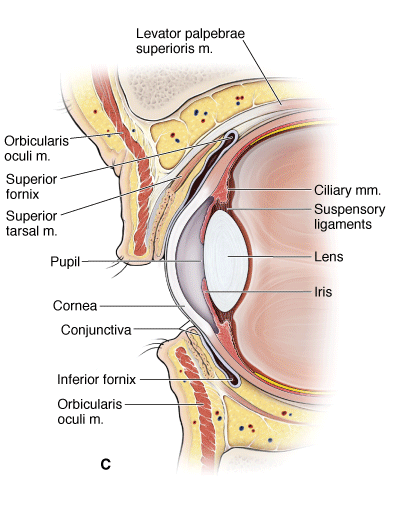 The external surface of the eyelids is covered by skin, whereas the conjunctiva covers the internal surface.
The external surface of the eyelids is covered by skin, whereas the conjunctiva covers the internal surface.
Conjunctiva
The conjunctiva is a mucous membrane that lines the internal surface of the eyelids. The conjunctiva is reflected at the superior and inferior fornices onto the anterior surface of the eyeball and forms the conjunctival sac when the eyes are closed.
Eyelid Muscles
Tears produced by the lacrimal gland are secreted continually and are spread over the conjunctiva and cornea by movement of the eyelids (blinking). The following muscles are involved in movement of the eyelids:
- Orbicular oculi muscle. Considered a muscle of facial expression. Its circular fibers attach to the anterior surface of the bony orbit as well as in the eyelid. When the facial nerve (CN VII) activates the orbicular oculi muscle, the eyes close.
-
The facial or seventh nerve innervates the circumferential orbicularis oculi to close the upper and lower eyelids.
An additional accessory smooth muscle, Müller's muscle, is innervated by the sympathetic nervous system. It arises from the undersurface of the levator palpebrae superioris and inserts into the superior tarsus. It contributes approximately 1 to 2 mm to the elevation of the upper eyelid (figure 1)
Oblique section through the upper and lower eyelids From: Smith's Ophthalmic Plastic and Reconstructive Surgery, 2nd ed, Mosby, St. Louis 1998. Copyright © 1998 Frank A Nesi, MD and Richard D Lisman, MD.
From: Smith's Ophthalmic Plastic and Reconstructive Surgery, 2nd ed, Mosby, St. Louis 1998. Copyright © 1998 Frank A Nesi, MD and Richard D Lisman, MD.Müller's muscle contributes to the over-elevation of the eyelid when a patient becomes excited or fearful and leads to mild ptosis with fatigue or inattention.
-
 The corneal, or blink, reflex is elicited by stimulation of the cornea. The nasociliary nerve (CN V-1) mediates the sensory portion of this reflex, with CN VII initiating the motor response by innervating the orbicularis oculi muscle.
The corneal, or blink, reflex is elicited by stimulation of the cornea. The nasociliary nerve (CN V-1) mediates the sensory portion of this reflex, with CN VII initiating the motor response by innervating the orbicularis oculi muscle.
- Levator palpebrae superioris muscle. The levator palpebrae superioris muscle elevates the upper eyelid and is innervated by CN III.
- The oculomotor or third cranial nerve innervates the levator palpebrae superioris to elevate the upper eyelid. The levator palpebrae superioris becomes a tendinous aponeurosis, which fuses with the anterior superior portion of the superior tarsal plate and possibly the pretarsal skin (see Figure above). This junction of the aponeurosis to the tarsus and orbicularis oculi forms the eyelid crease [1].
- Superior tarsal (Müller's) muscle. Composed of smooth muscle and attaches to the inferior surface of the levator palpebrae superioris muscle and the upper eyelid. These two muscles work synergistically to keep the eyelid elevated. The superior tarsal muscle is innervated by postganglionic sympathetic neurons that originate in the superior cervical ganglion and are carried to the orbit by the internal carotid and ophthalmic arteries.
 Horner's syndrome is caused by damage to the sympathetic innervation to the head (Figure 18-1D). Signs of Horner's syndrome found on the ipsilateral side of the injury include the following:
Horner's syndrome is caused by damage to the sympathetic innervation to the head (Figure 18-1D). Signs of Horner's syndrome found on the ipsilateral side of the injury include the following:
- Ptosis (drooping upper eyelid). Results from the loss of sympathetic innervation to the superior tarsal muscle.
- Anhidrosis (decreased sweating). Results from the loss of sympathetic innervation to sweat glands.
- Miosis (constricted pupil). Results from the loss of sympathetic innervation to the dilator pupillary muscle.

