USMLE Reviewer
(By Subscription)
Structure and Function
++++++++++++++++++++++
In contrast to a lobule, an acinus, the functional unit of the liver, is defined by a portal tract in the middle and centrilobular veins at the periphery.
Cells closest to the portal tract (zone 1) are well oxygenated; those closest to centrilobular veins (zone 3) receive the least oxygen and are most susceptible to injury.
Blood from hepatic arterioles and portal venules comingle in the sinusoidal channels, which lie between the cellular plates and serve as capillaries. These channels are lined by endothelial cells and by macrophages known as Kupffer cells. The Kupffer cells remove bacteria endotoxins, viruses, proteins and particulate matter from the blood. The space of Disse lies between the sinusoidal capillaries and the hepatocytes. Venous drainage from the central veins of hepatic lobules coalesces to form the hepatic veins (right, middle, and left), which empty into the inferior vena cava (Figure 32-2). The caudate lobe is usually drained by its own set of veins.

Hepatic blood flow. (Modified and reproduced, with permission, from Guyton AC: Textbook of Medical Physiology, 7th ed. W.B. Saunders, 1986.)
Bile canaliculi originate between hepatocytes within each plate and join to form bile ducts. An extensive system of lymphatic channels also forms within the plates and is in direct communication with the space of Disse.
The liver is supplied by sympathetic nerve fibers (T6-T11), parasympathetic fibers (right and left vagus), and fibers from the right phrenic nerve. Some autonomic fibers synapse first in the celiac plexus, whereas others reach the liver directly via splanchnic nerves and vagal branches before forming the hepatic plexus. The majority of sensory afferent fibers travel with sympathetic fibers.
The liver parenchyma has functional units called lobules. Each lobule is 1–2 mm in diameter and is made up of a maze-like arrangement of interconnected plates of hepatocytes separated by endothelium-lined sinusoids. The liver cell plates are arranged radially around the central vein; the liver cells that surround a portal tract comprise the limiting plate. Liver cell plates are normally one hepatocyte in thickness. Individual hepatocytes are large, with a central round nucleus, a prominent nucleolus, and abundant granular cytoplasm.

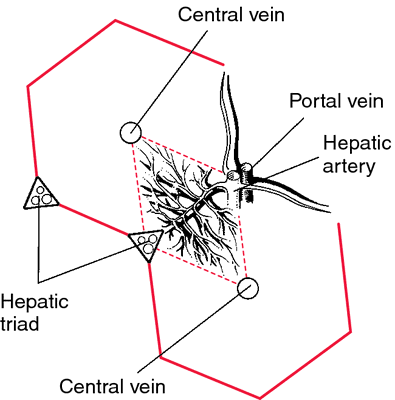
The sinusoids receive blood from branches of the portal vein and hepatic artery and drain into the central vein (solid arrows). Bile drainage is in the opposite direction, toward the portal tracts (dotted arrows).
The blood passes through sinusoids lined by single-layered sheets of hepatocytes. The sinusoids are fenestrated, allowing easy access of the products of digestion into hepatocytes. The sinusoids drain into central veins, which empty into the hepatic veins and finally to the IVC.
|
The portal triad is the triad of hepatic artery, portal vein, and bile duct. Portal triads form the six points of a hexagon that make up the liver lobule(See Figure Below).
In the portal triad, blood drains toward the central veins. Bile drains toward the bile ducts.
Bile secreted here passes through the interlobular ductules (canals of Hering) and the lobar ducts and then into the hepatic duct in the hilum. In most cases, the common hepatic duct is formed by the union of a single right and left duct, but in 25% of individuals, the anterior and posterior divisions of the right duct join the left duct separately. The origin of the common hepatic duct is close to the liver but always outside its substance. It runs about 4 cm before joining the cystic duct to form the common bile duct. The common duct begins in the hepatoduodenal ligament, passes behind the first portion of the duodenum, and runs in a groove on the posterior surface of the pancreas before entering the duodenum. Its terminal 1 cm is intimately adherent to the duodenal wall. The total length of the common duct is about 9 cm.1 Numerous microvilli increase the canalicular surface area.
The liver produces bile, which emulsifies fat.
Protein Production: clotting factor production, The liver is the source of plasma albumin; many plasma globulins, including alpha 1-antitrypsin (alpha-antiprotease); and many proteins of the coagulation cascade.
B. Fat Metabolism
Free fatty acids from adipose tissue and medium- or short-chain fatty acids absorbed in the intestine are brought to the liver. Triglycerides, cholesterol, and phospholipids are synthesized in the liver from the fatty acids and complexed with specific lipid acceptor proteins to form very-low-density lipoproteins that enter the plasma. The liver also metabolizes intermediate- and low-density lipoproteins.
C. Cholesterol Metabolism
Protein Metabolism
In addition to its synthetic function, the liver is the central organ in protein catabolism and synthesis of urea. Urea is secreted by the liver into the plasma for excretion by the kidney.
The liver plays a role in detoxifying noxious nitrogenous compounds derived from the intestine, as well as many drugs and chemicals.
Second, the blood flow draining the intestine is arranged such that substances that are absorbed pass first through the liver, allowing for the removal and metabolism of any toxins that have inadvertently been taken up, as well as clearance of particulates, such as small numbers of enteric bacteria.
The liver plays a vital role in detoxifying noxious nitrogenous compounds derived from the intestine, as well as many drugs and chemicals.
Phagocytosis via the Kupffer cells lining the sinusoids
The liver filter aged and damaged blood cells from the blood.
Bilirubin, cholesterol, urobilinogen, and bile acids excreted by the liver in bile, thence into the intestine to be excreted with the feces.
The liver is made up of discrete anatomic units called lobules. Each lobule is composed of plates of hepatocytes arranged cylindrically around a centrilobular vein. Four to five portal tracts, composed of hepatic arterioles, portal venules, bile canaliculi, lymphatics, and nerves, surround each lobule.
The hepatic lobule.
In contrast to a lobule, an acinus, the functional unit of the liver, is defined by a portal tract in the middle and centrilobular veins at the periphery. Cells closest to the portal tract (zone 1) are well oxygenated; those closest to centrilobular veins (zone 3) receive the least oxygen and are most susceptible to injury.
Blood from hepatic arterioles and portal venules comingle in the sinusoidal channels, which lie between the cellular plates and serve as capillaries. These channels are lined by endothelial cells and by macrophages known as Kupffer cells. The Kupffer cells remove bacteria endotoxins, viruses, proteins and particulate matter from the blood. The space of Disse lies between the sinusoidal capillaries and the hepatocytes. Venous drainage from the central veins of hepatic lobules coalesces to form the hepatic veins (right, middle, and left), which empty into the inferior vena cava (Figure 32-2). The caudate lobe is usually drained by its own set of veins.
Hepatic blood flow. (Modified and reproduced, with permission, from Guyton AC: Textbook of Medical Physiology, 7th ed. W.B. Saunders, 1986.)
Bile canaliculi originate between hepatocytes within each plate and join to form bile ducts. An extensive system of lymphatic channels also forms within the plates and is in direct communication with the space of Disse.
The liver is supplied by sympathetic nerve fibers (T6-T11), parasympathetic fibers (right and left vagus), and fibers from the right phrenic nerve. Some autonomic fibers synapse first in the celiac plexus, whereas others reach the liver directly via splanchnic nerves and vagal branches before forming the hepatic plexus. The majority of sensory afferent fibers travel with sympathetic fibers.
The liver parenchyma has functional units called lobules. Each lobule is 1–2 mm in diameter and is made up of a maze-like arrangement of interconnected plates of hepatocytes separated by endothelium-lined sinusoids. The liver cell plates are arranged radially around the central vein; the liver cells that surround a portal tract comprise the limiting plate. Liver cell plates are normally one hepatocyte in thickness. Individual hepatocytes are large, with a central round nucleus, a prominent nucleolus, and abundant granular cytoplasm.
The sinusoids receive blood from branches of the portal vein and hepatic artery and drain into the central vein (solid arrows). Bile drainage is in the opposite direction, toward the portal tracts (dotted arrows).
The blood passes through sinusoids lined by single-layered sheets of hepatocytes. The sinusoids are fenestrated, allowing easy access of the products of digestion into hepatocytes. The sinusoids drain into central veins, which empty into the hepatic veins and finally to the IVC.
The liver cells are separated from the sinusoids by a narrow space (space of Disse) that contains connective tissue and represents the scant interstitial compartment of the liver.
Specialized cells of the macrophage system (Kupffer cells) are present in the sinusoids scattered among the endothelial cells.
The portal triad is the triad of hepatic artery, portal vein, and bile duct. Portal triads form the six points of a hexagon that make up the liver lobule(See Figure Below).
In the portal triad, blood drains toward the central veins. Bile drains toward the bile ducts.
A, Hepatic vasculature. B, The portal triad and the hepatic lobule. C, Histologic view of the portal triad and hepatic lobule.
Bile secreted here passes through the interlobular ductules (canals of Hering) and the lobar ducts and then into the hepatic duct in the hilum. In most cases, the common hepatic duct is formed by the union of a single right and left duct, but in 25% of individuals, the anterior and posterior divisions of the right duct join the left duct separately. The origin of the common hepatic duct is close to the liver but always outside its substance. It runs about 4 cm before joining the cystic duct to form the common bile duct. The common duct begins in the hepatoduodenal ligament, passes behind the first portion of the duodenum, and runs in a groove on the posterior surface of the pancreas before entering the duodenum. Its terminal 1 cm is intimately adherent to the duodenal wall. The total length of the common duct is about 9 cm.1 Numerous microvilli increase the canalicular surface area.